Health disparities, which have been exacerbated by the COVID-19 pandemic, have become a growing public health concern nationwide. There are also rising disparity concerns in home health care, one of the fastest growing health care sectors within the United States.
The number of homebound individuals who need care in the home is expected to grow rapidly in size, complexity and diversity in both rural and urban areas. This is anticipated for several reasons: a rapidly aging American population, the strong preference of older adults and their families for aging in place, health policies that encourage the use of home- and community-based services, and the changing demographic profile of the American population, with substantial increases in racial and ethnic minorities.
As the role of homecare in the health care system grows, researchers are working to better understand how quality varies and whether there are disparities in care based on location, with a goal of optimizing home health care quality and reducing health disparities.
In 2018, more than 5 million Medicare beneficiaries received home health care. Of those recipients, about 9% were rural residents that were served by approximately 1,690 home health agencies located in rural areas, according to statistics reported on the home health care sector.
We recently published a longitudinal study analyzing national data on home health quality performance measures from the Centers for Medicare & Medicaid Services over five years (2014 to 2018) to understand differences in care quality between urban and rural home health agencies. The complete findings are published in the Journal of Rural Health.
Data in this study included 7,908 home health agencies nationwide, of which nearly 20% were in rural areas. The study measured home health agency quality and performance by looking at timely initiation of care (a measure of care processes) and hospitalization and emergency department visits (two measures of care outcomes). We discovered a number of differences between urban and rural agencies both at individual points in time and over the five year period that we studied.
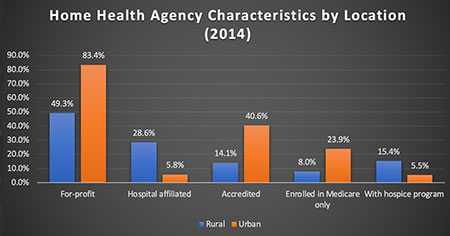
As Chart 1 shows, rural agencies were less likely than those in urban areas to be for-profit organizations and accredited. They were also more likely to be hospital based, enrolled in both Medicare and Medicaid programs and to offer hospice programs.
Compared to urban agencies, rural agencies consistently performed better on initiating care in a timely fashion, meaning that they quickly started home health care upon a doctor’s order or within two days of hospital discharge or referral to home health care (Figure 1). On average, rural agencies had a 1.05% higher annual rate of timely initiation of care, ranging from .88% higher in 2015 to 1.20% higher in 2017.
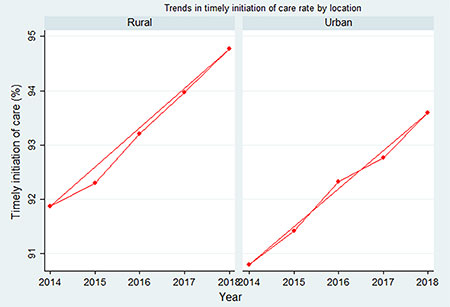
Figure 1. Trends in timely initiation of care rate: urban vs. rural
Rural: Urban:
2014: 91.89±6.74, range: 20.80-100.00 2014: 90.79±8.38, range: 20.00-100.00
2018: 94.78±6.79, range: 44.10-100.00 2018: 93.65±8.15, range: 17.20-100.00
Urban agencies consistently performed better on preventing hospitalization and emergency room visits during home health care overtime (Figure 2). Across the five years studied, urban agencies had an average of a .90% lower rate of hospitalization, ranging from .62% lower in 2017 to 1.27% lower in 2014. Urban agencies also had an average of 2.6% lower rate of emergency department visits, ranging from 2.48% lower in 2016 to 2.65% lower in 2014 (Figure 3).
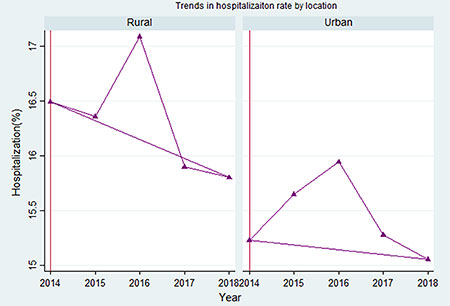
Figure 2. Trends in hospitalization rate: urban vs. rural
Rural: Urban:
2014: 16.52±3.99, range: 3.90-37.20 2014: 15.33±3.62, range: 0.90-40.20
2016: 17.05±3.99, range: 1.40-35.50 2016: 15.99±3.68, range: 0.00-41.10
2018: 15.79±3.82, range: 2.40-36.00 2018: 15.11±3.57, range: 0.00-38.40
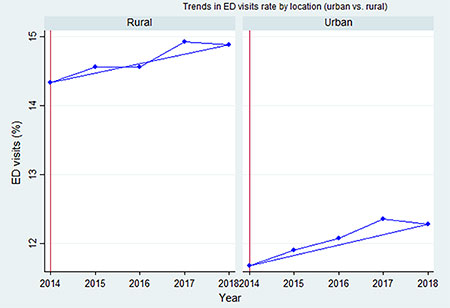
Figure 3. Trends in emergency department (ED) visits rate: urban vs. rural
Rural: Urban:
2014: 14.30±4.17, range: 2.00-45.70 2014: 11.71±3.70, range: 0.00-31.70
2018: 14.90±4.15, range: 0.60-38.90 2018: 12.28±3.82, range: 0.00-33.00
Importantly, the differences between rural and urban agencies were steady over time except for the gap in hospitalization rate, which narrowed slightly from a difference of 1.19% in 2014 to .68% in 2018. It should also be noted that the rate of emergency department visits increased over the five-year study period for both settings.
This study underscores the persistence of disparities in quality within home health care, related to both care processes and outcomes. The differences in rural and urban disparities in care processes and outcomes also indicate that agencies may choose different strategies given the resources they have and the care or client populations.
This study highlights the importance of considering the unique geographic, staffing and health challenges facing agencies when making investment to reduce rural-urban disparities. For instance, while rural agencies are more likely to have a better relationship with referring care facilities for faster initiation of care, they are often more restrained by staffing and the long commutes providers must make to reach patients’ homes. In addition, rural residents are in poorer health overall compared to their urban counterparts.
It is critically important for policymakers to consider such distinctive challenges to rural and urban agencies when making policies that aim to improve quality of home health care. There needs to be more opportunities for rural and urban agencies to share their strengths and learn from each other to figure out what really works.







